Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Lightning Injuries: 2014 Update

Chris Davis, MD; Anna Engeln, MD; Eric L. Johnson, MD; Scott E. McIntosh, MD, MPH; Ken Zafren, MD; Arthur A. Islas, MD, MPH; Christopher McStay, MD; William R. Smith, MD; Tracy Cushing, MD, MPH
From the Department of Emergency Medicine, University of Colorado School of Medicine, Aurora, CO (Drs Davis, McStay, and Cushing); the Department of Emergency Medicine, Denver Health Medical Center/University of Colorado School of Medicine, Denver,Colorado (Dr Engeln); the Department of Wound Healing and Hyperbaric Medicine, St. Alphonsus Hospital, Boise, ID, and Emergency Services, Teton Valley Hospital, Driggs, ID (Dr Johnson); the Division of Emergency Medicine, University of Utah School of Medicine, Salt Lake City, UT (Dr McIntosh); the Division of Emergency Medicine, Stanford University Medical Center, Palo Alto, CA, the Department of Emergency Medicine, Alaska Native Medical Center, Anchorage, AK, and the International Commission for Mountain Emergency Medicine (Dr Zafren); the Department of Family & Community Medicine, Paul L. Foster School of Medicine (Dr Islas); and the Department of Emergency Medicine, University of Washington School of Medicine, Seattle, WA, Department of Emergency Medicine, St. John’s Medical Center, Jackson, WY (Dr Smith).
To provide guidance to clinicians about best practices, the Wilderness Medical Society (WMS) convened an expert panel to develop evidence-based guidelines for the treatment and prevention of lightning injuries. These guidelines include a review of the epidemiology of lightning and recommendations for the prevention of lightning strikes, along with treatment recommendations organized by organ system. Recommendations are graded on the basis of the quality of supporting evidence according to criteria put forth by the American College of Chest Physicians. This is an updated version of the original WMS Practice Guidelines for Prevention and Treatment of Lightning Injuries published inWilderness & Environmental Medicine2012;23(3):260–269.
Key words:lightning, lightning strike, lightning injury, Lichtenberg, keraunoparalysis
Introduction
Lightning occurs nearly 50 times per second worldwide.^1 Approximately one-fifth of these flashes result in ground strikes. Internationally, an estimated 24,000 fatalities with 10 times as many injuries occur annually as a result of lightning.^2 ,^3 To provide guidance to clinicians and prehospital providers and to disseminate knowledge in this area, the Wilderness Medical Society (WMS) convened an expert panel to develop evidence-based guidelines for the treatment and prevention of lightning injuries. The WMS previously published guidelines on lightning injuries in 2006 and 2012.^4 ,^5 This is an updated version of the original WMS Practice Guidelines for Prevention and Treatment of Lightning Injuries published in Wilderness & Environmental Medicine 2012;23(3): 260 – 269. The goal of this review is to update the guidelines published in 2012 with relevant evidence- based information including a summary table of the best available literature. However, it must be recognized that the nature of lightning injuries often limits the available evidence to case reports and case series.
Methods
A panel was first convened at the 2011 Annual Meeting of the WMS in Snowmass, CO. Members were selected on the basis of clinical or research experience. The lead author identified articles through the PUBMED databases using a key word search with the terms lightning, lightning strike, lightning injury, Lichtenberg, and keraunoparalysis. This was supplemented by a hand search of these articles. The amassed evidence was then reviewed and graded for quality by the panel. In August 2014 these guidelines were updated using a key word search of PUBMED for lightning-related articles from 2011 to 2014. The same search terms were used. This supplement also incorporates suggestions from readers related to the original publication. The panel used the American College of Chest Physicians (ACCP) classification scheme for grading evidence and recommendations^6 (see onlineSupplementary ACCP Table 1). Injuries and recommended treatment strategies are organized by organ system.
Epidemiology
REGIONAL CONSIDERATIONS: WEATHER AND GEOGRAPHY
Lightning strikes are not uniformly distributed around the Earth (Figure 1). Regions with frequent thunderstorms have more lightning strikes. Thunderstorms are formed by 3 atmospheric elements: moisture, warm air on the surface of the earth, and a lifting wind. As the warm, moisture- laden air is pushed upward by vertical updraft, it condenses and cools, forming cumulonimbus clouds. Water freezes into ice particles near the top of this cloud. It is believed that the movement of these ice particles forms an electrical gradient (or differential) that is eventually dis- charged as lightning.^1
In addition to prevailing weather patterns, geography is also a determining factor in the location and frequency of thunderstorms. Central Africa has the greatest incidence of lightning strikes because of its mountainous terrain coupled with moist airflow from the Atlantic Ocean. This leads to year-round thunderstorms.^7 Worldwide, rural populations have been at greatest risk. Demographically this risk has been attributed to higher occupational exposure (rural farmers). These populations typically do not have access to substantial buildings that could provide shelter.^2 Though rare, lightning is possible even if the overlying sky is blue (so-called bolt from the blue).^8 This occurs in sunny conditions, usually after a storm,when strikes can return to areas from which the storm has passed, posing a risk to people who return to outdoor activity too soon. Lightning is also possible in snowstorms. Graupel (snow pellets) heralds weather favorable to lightning formation, as ice and snow pellets are believed to generate positive and negative charges as they collide, ultimately providing the electrical gradient that facilitates lightning formation.^9
TRENDS IN THE UNITED STATES
The incidence of lightning-related deaths in the United States has declined consistently during the past 50 years to approximately 40 deaths per year.^10 An estimated 400 lightning injuries occur annually based on data averaged over the last decade.^10 In comparison, approximately 70 flood-related deaths and 30 avalanche-related deaths occur yearly.^11 ,^12 A demographic study of lightning victims reveals that greater than 80% of victims are male.^13 Most deaths occur in individuals 20 to 45 year of age.^14 More than 90% of incidents occur between May and September.^14 Florida and Texas have accounted for nearly a quarter of all lightning-related deaths.^14 Lightning fatalities per state are reported inFigure 2. In the United States, the lifetime risk of being struck by lightning is estimated at 1:10,000.^10
Physics and Physiology
Lightning can be both negatively and positively charged and can take the form of both direct and alternating current depending on circumstance. However, lightning does not cause the muscle tetany seen with alternating currents of other electrical injuries. A bolt of lightning has a massive current ranging from 30,000 to 110,000 A, although such currents are only applied for 10 to 100 ms.^15 Energy transfer to the body is therefore limited.
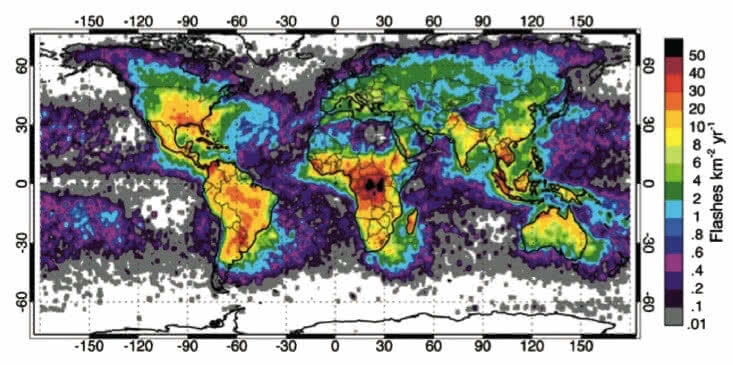
Figure 1.Worldwide density of lightning strikes.
Lightning injuries are classified as direct strike, contact injury, side splash, or ground current.^15 A direct strike occurs when there is an uninterrupted connection between a lightning bolt and an individual; direct strikes are relatively rare, accounting for approximately 5% of lightning strikes involving people.^15 Contact injury occurs when a person is touching an object that is struck. Side splash accounts for one-third of lightning injuries and occurs when the current“splashes”or jumps from a nearby object to the recipient’s body; such splashes follow the path of least resistance when compared with the initially struck object such as a tree. Ground current, also known as step voltage, occurs when lightning strikes an object or the ground near a person and travels through the ground from the strike point to the victim. This mechanism accounts for nearly half of lightning injuries.^15 A fifth mechanism of lightning injury has been recently reported. The“upward streamer” describes current passing up from the ground, through the victim, without a nearby ground strike; ultimately it is postulated that such a current does not become part of a completed lightning channel.^16 Lightning electricity, as with all electrical energy, will travel the path of least resistance. In body tissues, the order of least to greatest resistance is:
- nerve
- blood
- muscle
- skin
- fat
- bone.
Prevention
Evidence-based guidelines are limited regarding lightning prevention and safety. The following recommendations represent opinion from this panel or from previously published guidelines.^17 –^20
BEHAVIORAL STRATEGIES
No place is absolutely safe from lightning. However, individuals can choose safer places in an effort to reduce their risk of lightning strike.“When thunder roars, go indoors”is the currently recommended safety maxim of the National Weather Service. In essence, if one can hear thunder, then there is a risk of lightning strikes and one should seek shelter immediately. As substantial shelter is rarely available in the wilderness, hearing thunder in this setting should trigger an individual to immediately avoid or leave areas that are high risk for lightning strikes, such as ridgelines or summits, and to avoid tall objects such as ski lifts, cell phone towers, or isolated trees. One should observe for changing weather patterns that could indicate a developing thunderstorm: building cumulonimbus clouds, increasing winds, and darkening skies. Previous rules have relied on timing lightning flashes with thunder to estimate distance from an approaching storm. Such calculations may engender a false sense of security either from incorrect calculations or incorrect pairing of a given lightning flash with the correct thunderclap. Individuals should instead rely on observing signs of impending storms and seeking cover accordingly. Individuals should wait a minimum of 30 minutes after hearing the last thunderclap before resuming outdoor activity. Waiting 30 minutes should allow for the trailing edge of the thunder- storm to move the estimated 10 miles needed to establish an appropriate buffer zone. Recommendation grade: 1C.
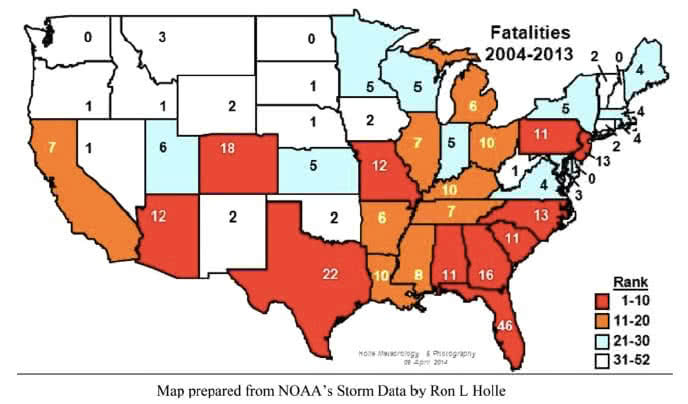
Figure 2. Lightning fatalities by state, 2004-2013.
SHELTER
There is no absolutely safe place from lightning—some locations are safer than others. When possible, shelter should be sought in the largest enclosed building available away from doors or windows. Another option is in a metal-topped vehicle with windows and doors closed; convertibles with fabric tops are not protective.^21 As this option is markedly limited in the wilderness setting, this panel recommends seeking a sheltered area inside a deep cave, far into a dense forest, or in a deep ravine; these features represent a safer alternative than remaining in an open, exposed area. Shallow caves, solitary trees, or open shelters (such as a picnic shelter, dugout, canopy, or lean-to) should be avoided because of the risk of side splash and ground current.^22 ,^23 Tents do not provide adequate protection from lightning.^24 When possible, the safest shelters are a building followed by a hardtop vehicle. Recommendation grade: 1C.
LIGHTNING POSITION
The lightning position involves sitting or crouching with knees and feet close together to create only one point of contact with the ground (Figure 3). If standing, have feet touching. If sitting, lift feet off the ground. Take this position only when a lightning strike is imminent and when all other lightning prevention strategies have failed. Signs of imminent strike include a blue haze around objects or individuals (St. Elmo’s fire), static electricity over hair or skin, an ozone smell, or a nearby crackling sound. Attempt to minimize the risk of ground current injury by insulating oneself from the ground; sit on a pack (remove any metal from the pack), a dry coiled rope, or a rolled foam sleeping pad. This is a strategy of last resort, as it is a difficult position to maintain for a long time, and should not be relied on as primary prevention but may reduce the risk of injury from an imminent lightning strike.^25 Recommendation grade: 2C.
GROUP SAFETY
This panel recommends the separation of group members by greater than 20 feet or more to limit potential mass casualties, as lightning can jump up to 15 feet between objects. Although each individual should be aware of lightning safety, groups should develop a specific light- ning safety plan. Such a plan accounts for local weather patterns, current weather forecast, local terrain, and predetermined available shelter and evacuation routes.^18 ,^19 A preestablished plan should mitigate the chaos of evacuating a crowd during a lightning storm. Further examples of lightning safety plans are available online through the National Lightning Safety Institute and the National Weather Service.^20 ,^26 Recommendation grade: 1C.
LIGHTNING DETECTION TECHNOLOGY
In the United States numerous commercial services are available that can provide automatic notifications when nearby lightning is detected by the National Lightning Detection Network (NLDN).^27 ,^28 Automatic notices of lightning activity are transmitted by e-mail, text, or cell phone to a predetermined individual. As cell phone reception is rarely available in the wilderness, personal lightning detection devices are an alternative option that does not rely on cellular technology. These devices are about the size of a pager, are easy to carry, and can detect lightning as far away as 75 miles. The device immediately signals the person of lightning activity and its distance by beeps, flashing lights, or a text message. This technology can be used to augment (but not supersede) a lightning safety plan. It should be noted that the available data on the efficacy of this technology is not peer reviewed and are largely based on manufacturer testimonials. Recommendation grade: 2C.
LIGHTNING IN A MOUNTAIN ENVIRONMENT
The panel strongly recommends the avoidance of peaks and ridgelines in the afternoon as thunderstorms are most frequent during this time period.^29 A common safety adage is “up by noon and down by two,” meaning that hikers and climbers should be off peaks and ridgelines by 2:00PM. If caught in a thunderstorm, climbers should tie-off individually as lightning is able to conduct over wet climbing ropes and may affect both climber and belayer. Individuals should discard metal objects such as ski poles or mountaineering axes to avoid contact burns.

Figure 3.Lightning position. Recommendation grade: 1C.
LIGHTNING IN A WATER ENVIRONMENT
This panel recommends that individuals exit the water and seek shelter expeditiously if caught swimming during a lightning storm.When rafting or kayaking, move to shore and away from the water’s edge as soon as possible. When boating, seek shelter below deck after locking off the helm.^30 If no shelter is available below, tie into a lifeline. Recommendation grade: 1C.
Injuries and Treatment
TRIAGE AND RESUSCITATION
The mechanism of sudden death from lightning strike is simultaneous cardiac and respiratory arrest. The patho- physiology is classically described as an initial asystolic arrest caused by the simultaneous depolarization of all myocardial cells. Ventricular fibrillation may also be observed.^31 Cardiac automaticity, typically in the form of sinus bradycardia, precedes recovery of the respiratory system. As the medullary respiratory center remains paralyzed despite return of spontaneous circulation (ROSC), a second cardiac arrest may occur if ventilation is not supported. Animal models corroborate this paradigm.^32 Death is rare should a victim survive the initial lightning strike.^33
Reverse triage
As ROSC precedes resolution of respiratory arrest, a patient’s ventilation should be supported as soon as possible. This highlights the need for a“reverse triage” system for lightning victims in which priority is initially given to those individuals without vital signs or spontaneous respirations.^31 In instances of multiple lightning casualties, we recommend using a reverse triage strategy. Recommendation grade 1C.
Resuscitation
Victims of lightning strike do not carry residual electrical charge; it is, therefore, safe to resuscitate these individuals immediately should the scene otherwise be deemed safe. Basic and advanced life support algorithms, including trauma when appropriate, remain the standard of care.^34 ,^35 There are numerous case reports of survival with intact neurologic function in lightning victims who received immediate resuscitation; mortality from cardiac arrest is lower in the lightning victims when compared with cardiac arrest in the general population.^31 ,^33 ,^36 ,^37 We recommend following current advanced life support guidelines for lightning victims requiring resuscitation.^34 ,^35 Recommendation grade: 1B.
CARDIOVASCULAR
The effect of a lightning strike on the cardiovascular system is variable ranging from benign electrocardiographic (ECG) changes to sudden death. Cardiovascular collapse is more commonly associated with direct strikes, whereas more transient ECG changes are seen with contact strikes or ground current.^38 Initial cardiovascular effects can include ST elevation, prolongation of the QT interval, cardiomyopathy, atrial fibrillation, and elevated cardiac markers.^38 –^40 Most of these findings resolve within 3 days, although pericarditis may recur several months after the initial injury.^38 Although ST elevation may suggest a localizing vascular lesion, coronary angiography may be normal.^41 In one instance, a victim experienced cardiogenic shock and required an intraaortic balloon pump. However, her cardiac function normalized after 72 hours.^42 It is important to note that delayed-onset symptoms and ECG changes have been reported as far out as 3 days.^38 ,^43 Labile blood pressures and autonomic instability are possible after lightning strikes and may persist for weeks to months.^44 ,^45
Initial cardiac evaluation
Once evacuated, we recommend that high-risk patients (Table),^46 including those experiencing a direct strike or those complaining of chest pain or dyspnea, receive a screening ECG and echocardiography. Recommendation grade: 1C
Cardiac markers
Although elevated cardiac markers are commonly reported after lightning strike, such abnormalities are not typically prognostic and do not correlate with anatomic lesions. Routine screening of cardiac markers, therefore, has limited clinical utility.^38 ,^41 ,^47 Recommendation grade: 2C.
Admission criteria
Patients experiencing a direct strike or those with an abnormal screening ECG or echocardiogram should be monitored with telemetry for a minimum of 24 hours.^38 ,^42 ,^43 ,^48 Recommendation grade: 1C.
Table.High-risk indicators in lightning strike victims
- Suspected direct strike
- Loss of consciousness
- Focal neurologic complaint
- Chest pain or dyspnea
- Major trauma defined by Revised Trauma Scoreo 444
- Cranial burns, leg burns or burns 4 10% TBSA
- Pregnancy
TBSA, total body surface area.
Return precautions
As delayed or recurring cardiac injuries such as pericarditis or cardiomyopathy are possible,^38 discharged patients should be counseled to return should they exhibit new chest pain or dyspnea. Recommendation grade: 1C.
NEUROLOGIC
Neurologic injuries are common after lightning strike and range from the transient and incidental to life threatening. These injuries have been categorized on the basis of symptom onset and duration.^49 As treatment strategies are limited for permanent neurologic injury resulting from lightning strikes, long-term neurorehabilitation is often the sole treatment option for those with permanent disability.^50 ,^51
Transient neurologic symptoms with immediate onset
This group accounts for the majority of neurologic manifestations of lightning injury. These include loss of consciousness, seizure, headache, paresthesia or weakness, confusion, and memory loss.
Keraunoparalysis
Transient paralysis after lightning strike has been documented in numerous case reports and is postulated to result from an overstimulation of the autonomic nervous system, leading to vascular spasm.^33 ,^49 ,^52 Typically, lower limbs are affected more than upper limbs. Signs and symptoms include lack of pulse, pallor or cyanosis, and motor and sensory loss in the affected extremities. Keraunoparalysis typically resolves within several hours. As keraunoparalysis may mimic a pulse- less victim, be vigilant to check a central pulse before starting cardiopulmonary resuscitation.We recommend hospital observation for keraunoparalysis. This phenomenon typically resolves spontaneously but may indicate more serious underlying trauma.^49 Recom- mendation grade: 1C.
Keraunoparalysis can mimic a spinal injury; thus, spinal precautions should be maintained and diagnostic imaging should be performed to rule out spinal cord injury if neurologic deficits persist despite resolution of pallor or pulselessness.^33 Recommendation grade: 1C.
Permanent neurologic symptoms with immediate onset
Permanent neurologic injury can manifest immediately after lightning strike, such as hypoxic encephalopathy resulting from cardiopulmonary arrest.^49 Lightning- induced intracranial hemorrhage may also occur instantly, most commonly affecting the basal ganglia or brainstem; this is believed to be attributable to preferential conduction of electricity through these areas of the brain.^49 ,^53 ,^54 Direct strikes to the head demonstrated higher fatality rates when compared with indirect strikes in one series.^55 Less common immediate-onset permanent neurologic injuries include peripheral nerve lesions, cerebral infarction, and cerebral salt-wasting syndrome.^55 –^57
Delayed neurologic syndromes
A multitude of delayed neurologic syndromes have been reported in victims struck by lightning. However, causal- ity to lightning strike has not been clearly established and the underlying pathophysiology is not yet understood.^54 ,^58 –^60 Progressive myelopathy has been described, resulting in weakness or sensory loss in the weeks to months after initial injury.^49 ,^59 Both animal models and human case studies have demonstrated the highest incidence of damage in the cervical and thoracic regions of the spinal cord.^59 ,^61 We recommend that anyone with delayed neurologic symptoms seek follow-up and treatment recommendations from a neurologist as soon as medically feasible. Recommendation grade: 2C.
Central nervous system injuries associated with secondary trauma and blast effect Any person having been struck by lightning should have a thorough examination for traumatic head injuries. All lightning strike victims with loss of consciousness or a persistently abnormal neurologic examination should receive a computerized tomography scan of the head.^49 ,^62 Recommendation grade: 1C.
DERMATOLOGIC
Lichtenbergfigure
A transient “ferning” or “feathering” pattern known as the Lichtenbergfigure is pathognomonic for lightning strike. It is not a burn, although its pathogenesis remains controversial.^63 This finding generally presents within 1 hour of lightning strike, and resolves in less than 24 hours. No histological change or damage has been found on biopsy, although pigment changes in the deeper layers of the skin may persist.^64 Treatment for these figures is not required, but their presence requires evaluation for other effects of lightning strike. Recommendation grade: 1C.
Burns
Burns associated with lightning injury include linear burns, punctate burns, and full-thickness burns. Linear burns are typically partial-thickness burns that result as sweat vaporizes into steam when lightning travels over the skin (also known as“flashover”). Areas that have heavy sweat concentration such as the underarms and beneath the breasts tend to be most affected.^65 Punctate burns are clustered circular burns believed to be the result of current passing out from the underlying deep tissue. An example is the“tip-toe”sign; these are small (usually < 1 cm) full-thickness burns found at the distal toes or sole of the foot. These burns are thought to result from current exiting the body. Punctate burns can also be caused by water droplets on the skin (from sweat or rain) becoming superheated and turning to steam from the energy of a lightning strike. Larger full-thickness burns are typically found in areas where the skin is in direct contact with synthetic fabric that melts onto skin or a metal object that is heated by the electrical energy of the lightning strike.^66 Full-thickness burns requiring skin grafting are uncommon; only 10% of lightning victims required skin grafting in a case series of 16 patients treated in a burn unit.^67 It is worth noting that the presence of cranial burns predicted a 3-fold increase in mortality in one series, and these patients were twice as likely to undergo cardiac arrest.^33
In limited case series, superficial burns related to lightning that involve less than 20% of total body surface area tend to heal quickly and may be treated with routine burn care.^67 –^69 Recommendation grade: 1C. If caught in a storm, remove metal objects such as watches, belt buckles, and necklaces in an effort to limit contact burns.^66 Recommendation grade: 1C.
EYE
Ocular injuries are common after lightning strike and may affect the anterior and posterior chambers. Damage may result from a number of mechanisms, including passage of current through the lens, blunt and blast trauma, vaso- constriction, or heat. The lens is commonly injured after lightning strike. Cataracts, often bilateral, comprise the majority of these injuries although their exact incidence is not reliably known.^70 Cataracts have been observed to develop between 2 days and 4 years after injury.^70 –^72 Visual prognosis is dependent on the extent of irreversible retinal damage and optic nerve injury as well as cataract formation. Ophthalmology evaluation is essential for all survivors of a high-risk (Table) lightning strike and for any victim who develops vision loss as soon as medically feasible. Recommendation grade: 1C.
EAR
The audiovestibular system is vulnerable to lightning, as it is a low-resistance pathway.^73 Tympanic membrane (TM) rupture was present in more than 60% of subjects in one case series in which 12 of 18 lightning victims had ruptured TMs.^74 Rupture may occur through a combination of blast trauma and electrical injury. Uncomplicated TM rupture usually heals spontaneously and can be managed conservatively. Otorrhea may be a sign of underlying basilar skull fracture and secondary trauma. Sensorineural deafness is also common after lightning strike and is usually transient. However, passage of current through the temporal bone may cause microhemorrhages and microfractures to the deeper structures of the ear, resulting in permanent hearing loss.^74 Initial evaluation for TM integrity is necessary in all lightning strike victims; follow-up with an otolaryngologist is essential for victims with hearing loss. Recommendation grade: 1C.
PSYCHIATRIC AND NEUROCOGNITIVE
A number of poststrike psychiatric and cognitive dysfunctions are described in the literature.^50 ,^75 These are typically divided into functional or behavioral categories. Functional deficits include abnormalities in memory and concentration including a reduced capacity for problem solving. Behavioral problems include depression, sleep disturbances, emotional lability, and aggressive behavior. These syndromes typically develop in days to weeks after a lightning strike, usually after the individual has returned from the wilderness setting. Victims and their families can be referred to one of several lightning support networks that may provide further coun- seling on the long-term sequelae of lightning injury. (Lightning Strike and Electric ShockSurvivors International, Inc: http://www.lightning-strike.org;e-mail:info@lightning- strike.org; phone: (910) 346-4708.) The lightning strike victim and his or her family should be counseled by primary providers to watch for symptoms of neuropsychiatric dysfunction and should seek specialized care from a mental health professional should such symptoms manifest. Recommendation grade: 1C.
PREGNANCY
Lightning strikes in pregnancy are rare, with only 13 cases reported in the literature.^76 –^81 Among these vic- tims, maternal mortality is zero, although fetal mortality approaches 50%. The fetus is likely at higher risk than the mother because it is surrounded by highly conductive amnioticfluid.^78 In addition to primary electrical injury, lightning strikes have been reported to cause uterine rupture and induction of labor.^82 Pregnant women greater than 20 weeks’gestation who have been struck by lightning should be evacuated to a hospital for lightning-associated injury screening and fetal monitoring. In general, pregnancies less than 20 weeks are not considered viable and do not require fetal monitoring. Recommendation grade: 1C.
DISPOSITION AND EVACUATION
Individuals with high-risk indicators (Table) should be evacuated immediately after the scene is determined to be safe for rescuers. Lower-risk lightning injuries and other casualties should be triaged and evacuated based on their injuries and overall medical condition. Recommendation grade: 1C.
Conclusions
This article provides an updated summary of available evidence for the prevention and treatment of lightning injury. Although numerous case reports have been published since the original practice guidelines were released in 2012, the summary recommendations remain largely unchanged. Most available data continue to be based on small, retrospective case reports or series because the prospective study of lightning injuries is not logistically and ethically possible. Although the strength of the overall evidence is limited, the authors still believe that many recommendations can be strongly supported [1C] as there is little risk of associated harm. Improved reporting to a national or international data- base could help with future epidemiological studies. Consensus on injury classification systems would also simplify the reporting process and allow data to be more easily combined for future study. (Also see the online Supplementary Evidence Table 2.)
Supplementary tables
Supplementary ACCP Table 1 and Evidence Table 2 are available online at10.1016/j.wem.2014.05.004.
References
- National Oceanic and Atmospheric Administration. Light- ning Climatology. 2008. Available at: http://www.nssl. noaa.gov/primer/lightning/ltg_climatology.html. Accessed February 28, 2012.
- Holle R. Annual rates of lightning fatalities by country. 20th Annual International Lightning Detection Confer- ence. Tucson, AZ; April 21–23, 2008. Available at: http://www.vaisala.com/Vaisala%20Documents/Scientific% 20papers/Annual_rates_of_lightning_fatalities_by_country.pdf. Accessed October 29, 2014.
- Cherington M, Walker J, Boyson M, Glancy R, Hedegaard H, Clark S. Closing the gap on the actual numbers of lightning casualties and deaths. 11th Conference on Applied Climatology. Dallas, TX: American Meteorolog- ical Society; 1999:379–380.
- Forgey WW, Wilderness Medical Society, Wilderness Medical Society Practice Guidelines for Wilderness Emergency Care. 5th ed. Guilford, CT: Falcon Guide; 2006.
- Davis C, Engeln A, Johnson E, et al. Wilderness Medical Society practice guidelines for the prevention and treat- ment of lightning injuries. Wilderness Environ Med. 2012;23:260– 269.
- Guyatt G, Gutterman D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force.Chest. 2006;129:174– 181.
- Christian HJ.Global Frequency and Distribution of Light- ning as Observed From Space.American Geophysical Union; 2001.
- Cherington M, Krider EP, Yarnell PR, Breed DW. A bolt from the blue: lightning strike to the head.Neurology. 1997;48:683– 686.
- Cherington M, Breed DW, Yarnell PR, Smith WE. Light- ning injuries during snowy conditions.Br J Sports Med. 1998;32:333– 335.
- National Weather Service. Medical Aspects of Lightning. 2010. Available at: http://www.lightningsafety.noaa.gov/ medical.htm. Accessed February 15, 2012.
- National Oceanic and Atmospheric Administration. Weather Fatalities. 2011. Available at:http://www.nws. noaa.gov/om/hazstats.shtml. Accessed March 2, 2012.
- Colorado Avalanche Information Center. Avalanche Acci- dent Statistics. 2011. Available at:http://avalanche.state. co.us/acc/acc_stats.php. Accessed March 2, 2012.
- Centers for Disease Control and Prevention (CDC), Lightning-associated deaths—United States, 1980–1995. MMWR Morb Mortal Wkly Rep. 1998;47:391– 394.
- Adekoya N, Nolte KB. Struck-by-lightning deaths in the United States.J Environ Health. 2005;67(45–50):58.
- Cooper MH, Holle RL. Mechanisms of lightning injury should affect lightning safety messages. 21st Annual International Lightning Detection Conference. Orlando, FL; April 19–20, 2010. Available at:http://www.vaisala.com/ Vaisala%20Documents/Scientific%20papers/11.Cooper,% 20Holle.pdf. Accessed October 29, 2014.
- Cooper MA. Afifth mechanism of lightning injury.Acad Emerg Med. 2002;9:172– 174.
- Zafren K, Durrer B, Herry JP, Brugger H, ICAR and UIAA MEDCOM. Lightning injuries: prevention and on- site treatment in mountains and remote areas. Official guidelines of the International Commission for Mountain Emergency Medicine and the Medical Commission of the International Mountaineering and Climbing Federation (ICAR and UIAA MEDCOM).Resuscitation. 2005;65: 369 – 372.
- Zimmermann C, Cooper MA, Holle RL. Lightning safety guidelines.Ann Emerg Med. 2002;39:660– 664. 19.Cooper MA, Holle R, Lopez R. Recommendations for lightning safety.JAMA. 1999;282:1132– 1133.
- National Lightning Safety Institute. Personal lightning safety. 2012. Available at:http://www.lightningsafety.com/ nlsi_pls.html. Accessed March 2, 2012.
- Holle R. Lightning-caused deaths and injuries in the vicinity of vehicles. National Lightning Safety Insti- tute; 2009. Available at:http://www.lightningsafety.com/ nlsi_pls/lightning-caused-deaths-around-vehicles.pdf. Acc- essed October 29, 2014.
- Bandara K. Lightning hazards: impacts and responses of the public. 18th Annual International Lightning Detection Conference. Helsinki, Finland: Vaisala; 2004.
- Rakov VA. Lightning protection of structures and per- sonal safety. 2000 International Lightning Detection Conference. Tucson, AZ; November 7–8, 2000. Available at: http://www.w1npp.org/events/2011/2011-F~1/SAFETY/ LIGHTN
1.COM/LIGHTN4.PDF. Accessed October 29, 2014. - Zack F, Hammer U, Klett I, Wegener R. Myocardial injury due to lightning.Int J Legal Med. 1997;110:326– 328.
- Roeder W. Analysis of short notice outdoor lightning risk reduction and comments on why it should not be taught. Struck by Lightning. American Meteorological Society; 2008.
- National Weather Service. Lightning risk reduction. 2011. Available at: http://www.lightningsafety.noaa.gov/out doors.htm. Accessed March 2, 2012.
- Holle RH, Lopez RE, National Severe Storms Laboratory. Overview of Real-Time Lightning Detection Systems and Their Meteorological Uses.Norman, OK; Springfield, VA: U.S. Dept. of Commerce, National Oceanic and Atmos- pheric Administration, Environmental Research Laborato- ries, National Severe Storms Laboratory; for sale by the National Technical Information Service; 1993.
- Kithil R. An overview of lightning detection equipment. 2011. Available at: http://www.lightningsafety.com/ nlsi_lhm/overview2002.html. Accessed March 3, 2012.
- Vogt BJ. Visualizing summertime lightning patterns on Colorado fourteeners.Prof Geogr. 2012;66:41– 57.
- Becker W.Boating: Lightning Protection.Gainesville, FL: University of Florida; 1992.
- Taussig HB.“Death”from lightning and the possibility of living again.Am Sci. 1969;57:306– 316.
- Andrews CDM. Effects of lightning on mammalian tissue. Proceedings of the International Conference of Lightning and Static Electricity. Bath, England; 1989:104.
- Cooper MA. Lightning injuries: prognostic signs for death. Ann Emerg Med. 1980;9:134– 138.
- 2005 American Heart Association Guidelines for Cardio- pulmonary Resuscitation and Emergency Cardiovascular Care.Circulation. 2005;112(24 Suppl):IV1–IV203.
- Driscoll P, Wardrope J. ATLS: past, present, and future. Emerg Med J. 2005;22:2– 3.
- Courtman SP, Wilson PM, Mok Q. Case report of a 13- year-old struck by lightning. Paediatr Anaesth. 2003; 13:76– 79.
- Fahmy FS, Brinsden MD, Smith J, Frame JD. Lightning: the multisystem group injuries.J Trauma. 1999;46:937– 940.
- Lichtenberg R, Dries D, Ward K, Marshall W, Scanlon P. Cardiovascular effects of lightning strikes. J Am Coll Cardiol. 1993;21:531– 536.
- Jackson SH, Parry DJ. Lightning and the heart.Br Heart J. 1980;43:454– 457.
- Dronacahrya L, Poudel R. Lightning induced atrialfibril- lation.Kathmandu Univ Med J (KUMJ). 2008;6:514– 515.
- Saglam H, Yavuz Y, Yurumez Y, Ozkececi G, Kilit C. A case of acute myocardial infarction due to indirect light- ning strike.J Electrocardiol. 2007;40:527– 530.
- Rivera J, Romero KA, González-Chon O, Uruchurtu E, Márquez MF, Guevara M. Severe stunned myocardium after lightning strike.Crit Care Med. 2007;35:280– 285.
- Palmer AB. Lightning injury causing prolongation of the Q-T interval.Postgrad Med J. 1987;63:891– 894.
- Weeramanthri TS, Puddey IB, Beilin LJ. Lightning strike and autonomic failure—coincidence or causally related?J R Soc Med. 1991;84:687– 688.
- Grubb BP, Karabin B. New onset postural tachycardia syndrome following lightning injury.Pacing Clin Electro- physiol. 2007;30:1036– 1038.
- Champion HR, Sacco WJ, Copes WS, Gann DS, Gennar- elli TA, Flanagan ME. A revision of the Trauma Score.J Trauma. 1989;29:623– 629.
- Alyan O, Ozdemir O, Tufekcioglu O, Geyik B, Aras D, Demirkan D. Myocardial injury due to lightning strike—a case report.Angiology. 2006;57:219– 223.
- Dundon BK, Puri R, Leong DP, Worthley MI. Takotsubo cardiomyopathy following lightning strike.Emerg Med J. 2008;25:460– 461.
- Cherington M. Spectrum of neurologic complications of lightning injuries.NeuroRehabilitation. 2005;20:3– 8.
- Cherington M. Neurorehabilitation of the multifaceted and complicated neurologic problems associated with lightning and electrical injuries.NeuroRehabilitation. 2005;20:1– 2.
- Yarnell PR. Neurorehabilitation of cerebral disorders following lightning and electrical trauma.NeuroRehabili- tation. 2005;20:15– 18.
- ten Duis HJ, Klasen HJ, Reenalda PE. Keraunoparalysis, a ‘specific’lightning injury.Burns. 1985;l2:54– 57. 53.Cherington M. Lightning injuries. Ann Emerg Med. 1995;25:517– 519.
- Cherington M. Central nervous system complications of lightning and electrical injuries.Semin Neurol. 1995;15: 233 – 240.
- Kleinschmidt-DeMasters BK. Neuropathology of lightning-strike injuries.Semin Neurol. 1995;15:323– 328.
- Emet M, Caner I, Cakir M, Aslan S, Cakir Z. Lightning injury may cause abrupt cerebral salt wasting syndrome. Am J Emerg Med. 2010;28(640):e1–e3.
- Frayne JH, Gilligan BS. Neurological sequelae of light- ning stroke.Clin Exp Neurol. 1987;24:195– 200.
- Belsole RJ, Smith AA. Reflex sympathetic dystrophy: “gate”closed by lightning.J Hand Surg Am. 1990;15:523.
- Davidson GS, Deck JH. Delayed myelopathy following lightning strike: a demyelinating process. Acta Neuro- pathol. 1988;77:104– 108.
- O’Brien CF. Involuntary movement disorders following light- ning and electrical injuries.Semin Neurol. 1995;15:263– 267.
- Lakshminarayanan S, Chokroverty S, Eshkar N, Grewal R. The spinal cord in lightning injury: a report of two cases. J Neurol Sci. 2009;276:199– 201.
- Aslan S, Yilmaz S, Karcioglu O. Lightning: an unusual cause of cerebellar infarction.Emerg Med J. 2004;21:750– 751.
- Cherington M, McDonough G, Olson S, Russon R, Yarnell PR. Lichtenbergfigures and lightning: case reports and review of the literature.Cutis. 2007;80:141– 143.
- Resnik BI, Wetli CV. Lichtenbergfigures.Am J Forensic Med Pathol. 1996;17:99– 102.
- Cooper MA. Emergent care of lightning and electrical injuries.Semin Neurol. 1995;15:268– 278.
- Herrero F, García-Morato V, Salinas V, Alonso S. An unusual case of lightning injury: a melted silver necklace causing a full thickness linear burn.Burns. 1995;21:308– 309.
- Maghsoudi H, Adyani Y, Ahmadian N. Electrical and lightning injuries.J Burn Care Res. 2007;28:255– 261.
- Matthews MS, Fahey AL. Plastic surgical considerations in lightning injuries.Ann Plast Surg. 1997;39:561– 565.
- Selvaggi G, Monstrey S, Van Landuyt K, Hamdi M, Blondeel P. Rehabilitation of burn injured patients follow- ing lightning and electrical trauma.NeuroRehabilitation. 2005;20:35– 42.
- Sommer LK, Lund-Andersen H. Skin burn, bilateral iridocyclitis and amnesia following a lightning injury. Acta Ophthalmol Scand. 2004;82:596– 598.
- Espaillat A, Janigian R Jr, To K. Cataracts, bilateral macular holes, and rhegmatogenous retinal detachment induced by lightning.Am J Ophthalmol. 1999;127:216– 217.
- Cazabon S, Dabbs TR. Lightning-induced cataract.Eye (Lond). 2000;14(Pt 6):903– 904.
- Jones DT, Ogren FP, Roh LH, Moore GF. Lightning and its effects on the auditory system. Laryngoscope. 1991;101:830– 834.
- GluncićI, Roje Z, GluncićV, Poljak K. Ear injuries caused by lightning: report of 18 cases.J Laryngol Otol. 2001;115:4– 8.
- Primeau M, Engelstatter GH, Bares KK. Behavioral consequences of lightning and electrical injury. Semin Neurol. 1995;15:279– 285.
- Pierce MR, Henderson RA, Mitchell JM. Cardiopulmo- nary arrest secondary to lightning injury in a pregnant woman.Ann Emerg Med. 1986;15:597– 599.
- García Gutiérrez JJ, Meléndez J, Torrero JV, Obregón O, Uceda M, Gabilondo FJ. Lightning injuries in a pregnant woman: a case report and review of the literature.Burns. 2005;31:1045– 1049.
- Flannery DB, Wiles H. Follow-up of a survivor of intra- uterine lightning exposure. Am J Obstet Gynecol. 1982;142:238– 239.
- Weinstein L. Lightning: a rare cause of intrauterine death with maternal survival.South Med J. 1979;72:632– 633.
- Chan YF, Sivasamboo R. Lightning accidents in preg- nancy.J Obstet Gynaecol Br Commonw. 1972;79:761– 762.
- Rees WD. Pregnant Woman Struck by Lightning.BMJ. 1965;1:103– 104.
- Guha-Ray DK. Fetal death at term due to lightning.Am J Obstet Gynecol. 1979;134:103– 105.
