
ANZCOR GUIDELINE 9.2.5 – FIRST AID FOR ASTHMA
Guideline
Who does this guideline apply to?
This guideline applies to adult and child victims.
Who is the audience for this guideline?
This guideline is for use by bystanders, first aiders and first aid providers.
1 Introduction
Asthma is a disorder of the smaller airways of the lungs. People with asthma have sensitive airways which can narrow when exposed to certain ‘triggers’, leading to difficulty in breathing.
Three main factors cause the airways to narrow:
- The muscle around the airway tightens (bronchoconstriction).
- The inside lining of the airways becomes swollen (inflammation)
- Extra mucus (sticky fluid) may be produced.
In asthma, symptoms are made worse by 'triggers'. Every person's asthma is different and not all people will have the same triggers. Triggers can include:
- Respiratory infection
- Irritants (e.g. cigarette, wood fire or bushfire smoke, occasionally perfumed or cleaning products)
- Inhaled allergens (e.g. dust mite, mould spores, animal danders, grass/tree pollen)
- Cold air, exercise, laughing/crying
- Non steroidal anti-inflammatory agents (e.g. aspirin, ibuprofen)
- Sulfite additives (food preservatives) – more common in those with poorly controlled asthma
- Food allergy – while usually accompanied by other symptoms such as rash or vomiting, isolated severe asthma may occur as the only presentation and may result in death
- Food colours and flavours
- Emotional triggers such as stress.
Most fatal cases of food-induced anaphylaxis occur in those with asthma. In patients with asthma known to be at risk from anaphylaxis, if it is uncertain whether the patient is suffering from asthma or anaphylaxis, it is appropriate to administer an adrenaline autoinjector first, followed by asthma reliever medication. No harm is likely to occur by doing so in a patient having asthma without anaphylaxis.
2 Recognition
Asthma can be recognised by the following symptoms and signs:
- A dry, irritating, persistent cough, particularly at night, early morning, with exercise or activity
- Chest tightness
- Shortness of breath
- Wheeze (high pitched whistling sound during breathing).
2.1 Symptoms and signs of a severe asthma attack include some or all of the following:
- Gasping for breath (may have little or no wheeze due to little movement of air)
- Severe chest tightness
- Inability to speak more than one or two words per breath
- Feeling distressed and anxious
- Little or no improvement after using “reliever” medication
- ‘Sucking in’ of the throat and rib muscles, use of shoulder muscles or bracing with arms to help breathing
- Blue discolouration around the lips (can be hard to see if skin colour also changes)
- Pale and sweaty skin
- Symptoms rapidly getting worse or using reliever more than every two hours.2
As well as the above symptoms, young children appear restless, unable to settle or become drowsy. A child may also ‘suck’ in muscles around the ribs and may have problems eating or drinking due to shortness of breath. A child also may have severe coughing and vomiting.
An asthma attack can take anything from a few minutes to a few days to develop.
3 Managing An Asthma Attack
If the victim has a personal written asthma action plan then that plan should be followed.
If there is no action plan in place then use the following Asthma First Aid plan.
3.1 Asthma First Aid Plan
If a victim has any signs of a severe asthma attack, call an ambulance straight away and follow the Asthma First Aid Plan while waiting for the ambulance to arrive.
| Step | Australia (4 x 4 x 4) | New Zealand (6 x 6 x 6) |
|---|---|---|
| 1 | Sit the person comfortably upright. Be calm and reassuring. Do not leave the person alone. | Sit the person comfortably upright. Be calm and reassuring. Do not leave the person alone. |
| 2 | Without delay give four separate puffs of a “reliever”. The medication is best given one puff at a time via a spacer device. Ask the person to take four breaths from the spacer after each puff of medication. | Without delay give six separate puffs of a “reliever”. The medication is best given one puff at a time via a spacer device. Ask the person to take six breaths from the spacer after each puff of medication. |
| 3 | Wait four minutes. If there is little or no improvement give another four puffs. | Wait six minutes. If there is little or no improvement give another six puffs. |
| 4 | If there is still no improvement, call an ambulance immediately. Keep giving four puffs every four minutes until the ambulance arrives. | If there is still no improvement, call an ambulance immediately. Keep giving six puffs every six minutes until the ambulance arrives. |
If a spacer is not available, simply use the inhaler. Use the victim’s own inhaler if possible. If not,use the first aid kit inhaler if available or borrow one from someone else.
No harm is likely to result from giving a “reliever” inhaler to someone without asthma.2 [LOE: Expert Consensus Opinion].
If oxygen is available, it should be administered by a person trained in its use, following Use of Oxygen in Emergencies (ANZCOR Guideline 10.4). [LOE: Expert Consensus Opinion].
If a severe allergic reaction is suspected, follow Anaphylaxis – First Aid Management (ANZCOR Guideline 9.2.7)
If victim becomes unresponsive and not breathing normally, commence resuscitation following the Basic Life Support Flowchart (ANZCOR Guideline 8).
4 Regional differences in recommended dose and intervals
There are differences in first aid treatment recommendations (e.g. doses and timing of relievers) between Australia and New Zealand. Additionally treatment recommendations for the clinical management of acute asthma by health professionals are different again.
In Australia, the National Asthma Council Australia recommends taking 4 puffs every 4 minutes (4 x 4 x 4) 4, 5 whereas in New Zealand, the Asthma and Respiratory Foundation NZ recommend taking 6 puffs every 6 minutes6 (6 x 6 x 6).
The 2015 International Consensus on First Aid Science did not provide any update on dosage or interval between doses. This guideline is not intended to contradict current recommendations of peak asthma bodies in Australia or in New Zealand – the ANZCOR recommended treatment in 3.1 accounts for these regional differences. This guideline does not seek to alter first aid practice (with respect to dosage or timing of reliever medication)in either Australia or New Zealand.
WITH SPACER
Assemble the spacer. Remove inhaler cap and shake well. Place the inhaler upright into the spacer. Place the spacer mouthpiece into the victim’s mouth, between the teeth with the lips sealed around it. Press firmly on the inhaler to fire one puff into the spacer. Ask the victim to breathe in and out normally for four to six breaths via the spacer. Repeat this promptly until four to six puffs have been given. Remember to shake the inhaler before each puff.


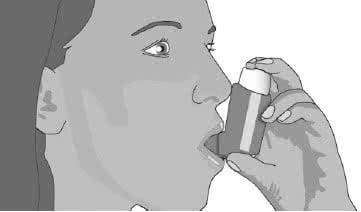
WITHOUT SPACER
When a spacer is unavailable, shake the inhaler. Place the mouthpiece into the victim’s mouth, between the teeth with the lips sealed around it. Press firmly on the inhaler to administer one puff as the victim inhales slowly and steadily. Slip the inhaler out of the victim’s mouth. Ask the victim to hold their breath for four seconds or as long as comfortable. Breathe out slowly away from the inhaler. Repeat this promptly until four to six puffs have been given. Remember to shake the inhaler before each puff.
The most common reliever medication is salbutamol. Victim’s own reliever medication may be used as an alternative.
References
- Asthma Australia. About asthma. https://www.asthmaaustralia.org.au/national/about-asthma Accessed 05/12/
- National Asthma Council Australia. Asthma Action Plans http://www.nationalasthma.org.au/health-professionals/asthma-action-plans Accessed 19/11/
- Zideman, D. A., Singletary, E. M., De Buck, E.,et al. (2015). Part 9: First aid: 2015 International Consensus on First Aid Science with Treatment Recommendations. Resuscitation, 95 , e225.http://www.cprguidelines.eu/assets/downloads/costr/S0300-9572(15)00368-8_main.pdf Accessed 19/11/
- National Asthma Council. First Aid for Asthma http://www.nationalasthma.org.au/first-aid Accessed 19/11/
- National Asthma Council Australia. Australian Asthma Handbook, Version 1.1. National Asthma Council Australia, Melbourne, 2015. Website. Available from: http://www.asthmahandbook.org.au Accessed 19/11/
- Asthma and Respiratory Foundation of New Zealand. Controlling your asthma [https://s3-ap-southeast- 2.amazonaws.com/assets.asthmafoundation.org.nz/documents/Controlling-Your-Asthma- Resource.pdf] Accessed 6/7/
Further Reading
ANZCOR Guideline 5 Breathing
ANZCOR Guideline 8 Cardiopulmonary Resuscitation
ANZCOR Guideline 9.2.7 Anaphylaxis – First Aid Management
ANZCOR Guideline 10.4 The Use of Oxygen in Emergencies