
ANZCOR Guideline 9.1.1 - First Aid for Management of Bleeding
Summary
Who does this guideline apply to?
This guideline applies to adults, children and infants.
Who is the audience for this guideline?
This guideline is for use by bystanders, first aiders and first aid training providers.
Recommendations
The Australian and New Zealand Committee on Resuscitation (ANZCOR) makes the following recommendations:
- Firm pressure on or around the wound is the most effective way to stop most bleeding. [Good Practice Statement]
- In life-threatening bleeding, control of bleeding takes priority over airway and breathing interventions. [Good Practice Statement]
- We suggest to use an arterial tourniquet for life-threatening limb bleeding that is not controlled by direct wound pressure.1 [CoSTR 2020, weak recommendation, very low certainty of evidence]
Abbreviations
ANZCOR: Australian and New Zealand Committee on Resuscitation CoSTR: Consensus on Science with Treatment Recommendations (from International Liaison Committee on Resuscitation - ILCOR) CPR: Cardiopulmonary Resuscitation
Guideline
1 External Bleeding
The use of pressure on or around the wound is usually the fastest, easiest and most effective way to stop external bleeding.1,2,3,4 [Good Practice Statement] Other methods should be used if direct pressure alone does not control severe bleeding. The aim is to stop further bleeding whilst waiting for help to arrive. There is no evidence that elevating a bleeding part will help control bleeding1,5 and there is the potential to cause more pain or injury.
Bleeding should be managed as severe, life-threatening bleeding in the following situations:
- amputated or partially amputated limb above wrist or ankle
- shark attack, propeller cuts or similar major trauma to any part of the body
- bleeding not controlled by local pressure
- bleeding with signs of shock, i.e. pale and sweaty plus pulse rate >100, or capillary refill > 2 sec and/or decreased level of consciousness
1.1 Management
- Use standard precautions (e.g. gloves, protective glasses) if readily available.
- Management of all bleeding begins with application of pressure on or around the wound.
- If bleeding is severe or life-threatening, controlling the bleeding takes priority over airway and breathing interventions. Lie the person down, apply pressure and call for an ambulance.
- If there is severe, life threatening bleeding from a limb, not controlled by pressure, we suggest to apply an arterial tourniquet above the bleeding point, if trained in its use and one is available.1 [CoSTR 2020: weak recommendation, very low certainty of evidence]
- If there is severe, life-threatening bleeding from a wound site not suitable for tourniquet, or from a limb when a tourniquet is not available or has failed to stop the bleeding, we suggest to apply a haemostatic dressing, if trained in its use and one is available.1,5 [CoSTR 2020: weak recommendation, low quality evidence]
- For the majority of non-life-threatening cases, first aiders should follow the sequence of DRSABCD, where control of bleeding follows establishing airway and commencing CPR if required.
- If the person is unresponsive and not breathing normally, follow the Basic Life Support Flowchart. [Refer to ANZCOR Guideline 8]
1.2 Direct Pressure Method
Where the bleeding point is identified, the rescuer, a bystander or the injured person should control bleeding by:
- Applying firm, direct pressure sufficient to stop the bleeding. Pressure can be applied using hands or a pad over the bleeding point.
- If bleeding continues, apply a second pad and a tighter bandage over the wound. If bleeding still continues, check that the pad and bandage are correctly applied, directly over the bleeding. If not, it may be necessary to remove the pad(s) to ensure that a specific bleeding point has not been missed. Applying firmer pressure, only using 1 to 2 pads over a small area, will achieve greater pressure over the bleeding point than continuing to layer up further pads.
To assist in controlling bleeding, where possible:
- Advise the person to lie down and remain still
- Restrict movement by immobilizing a bleeding limb
1.3 Embedded Objects
If there is an obvious embedded object causing bleeding, use pressure around the object. [ Good Practice Statement]
- Do not remove the embedded object because it may be plugging the wound and restricting bleeding.
- Apply padding around or on each side of the protruding object, with pressure over the padding.
Pressure application methods may be insufficient to control bleeding. It may still be necessary to use other measures including an arterial tourniquet or haemostatic dressings.
1.4 Arterial tourniquet
- Arterial tourniquets should only be used for life-threatening bleeding from a limb, where the bleeding cannot be controlled by direct pressure. Ideally, a tourniquet should not be applied over a joint or wound, and must not be covered up by any bandage or clothing.
- Commercially manufactured windlass tourniquets such as those based on military designs are more effective than improvised tourniquets1. An example of a military tourniquet is shown in Fig 1 below. Effective use of commercial tourniquets is optimal when first aid providers are trained in proper application techniques.
- All arterial tourniquets should be applied in accordance with the manufacturer's instructions (or 5 cm above the bleeding point if no instructions) and tightened until the bleeding stops.
- If a tourniquet does not stop the bleeding its position and application must be checked. Ideally the tourniquet is not applied over clothing nor wetsuits and is applied tightly, even if this causes local discomfort.
- If bleeding continues, a second tourniquet (if available) should be applied to the limb, preferably above the first.
- If a correctly applied tourniquet(s) has failed to control the bleeding consider using a haemostatic dressing in conjunction with the tourniquet.1,5 [Good Practice Statement]
- An elastic venous tourniquet (designed to assist drawing blood samples or inserting intravenous cannulae) is not suitable for use as an arterial tourniquet.
- Improvised tourniquets are unlikely to stop all circulation to the injured limb without risk of tissue damage. Improvised tourniquets which do not stop all circulation can increase bleeding. Nonetheless, in the context of life-threatening bleeding, an improvised tourniquet is likely to be better than no tourniquet. Tourniquets, ideally of a similar broad width to commercial types, can be improvised using materials from a first aid kit (e.g. triangular bandage, elastic bandage) from clothing, a surfboard leg rope or other available similar items. Improvised tourniquets should be tightened by twisting a rod or stick under the improvised tourniquet band, similar to the windlass in commercial tourniquets.
- The time of tourniquet application must be noted and communicated to emergency/paramedic personnel. Once applied, the person requires urgent transfer to hospital and the tourniquet should not be removed until the person receives specialist care.

Figure 1: Combat Application Tourniquet
1.5 Haemostatic dressings
- Haemostatic dressings are impregnated with agents that help stop bleeding. The haemostatic dressings included in the CoSTR 2015 recommendations contained the products kaolin and chitosan.6 They are commonly used to control bleeding in the surgical and military settings but their use in the civilian, non-surgical setting is becoming more common. An example is shown in Fig 2 below.
- When available and the first aid provider is trained in their use, we suggest that haemostatic dressings are of most value in the following situations [CoSTR 2015: weak recommendation, very low quality evidence]:5
- Severe, life-threatening bleeding not controlled by wound pressure, from a site not suitable for tourniquet use.
- Severe, life-threatening bleeding from a limb, not controlled by wound pressure, when the use of a tourniquet(s) alone has not stopped the bleeding, or a tourniquet is not available.
- Haemostatic dressings must be applied as close as possible to the bleeding point, held against the wound using local pressure (manually initially) then held in place with the application of a bandage (if available). Haemostatic dressings should be left on the bleeding point until definitive care is available.
The need to control the bleeding is paramount. The risks associated with the first aid use of tourniquets and haemostatic dressings are less than the risk of uncontrolled severe, life-threatening bleeding. These adjuncts provide temporary bleeding control and rapid transfer to hospital remains critically important.
Figure 2: Kaolin impregnated gauze (an example of a haemostatic dressing)
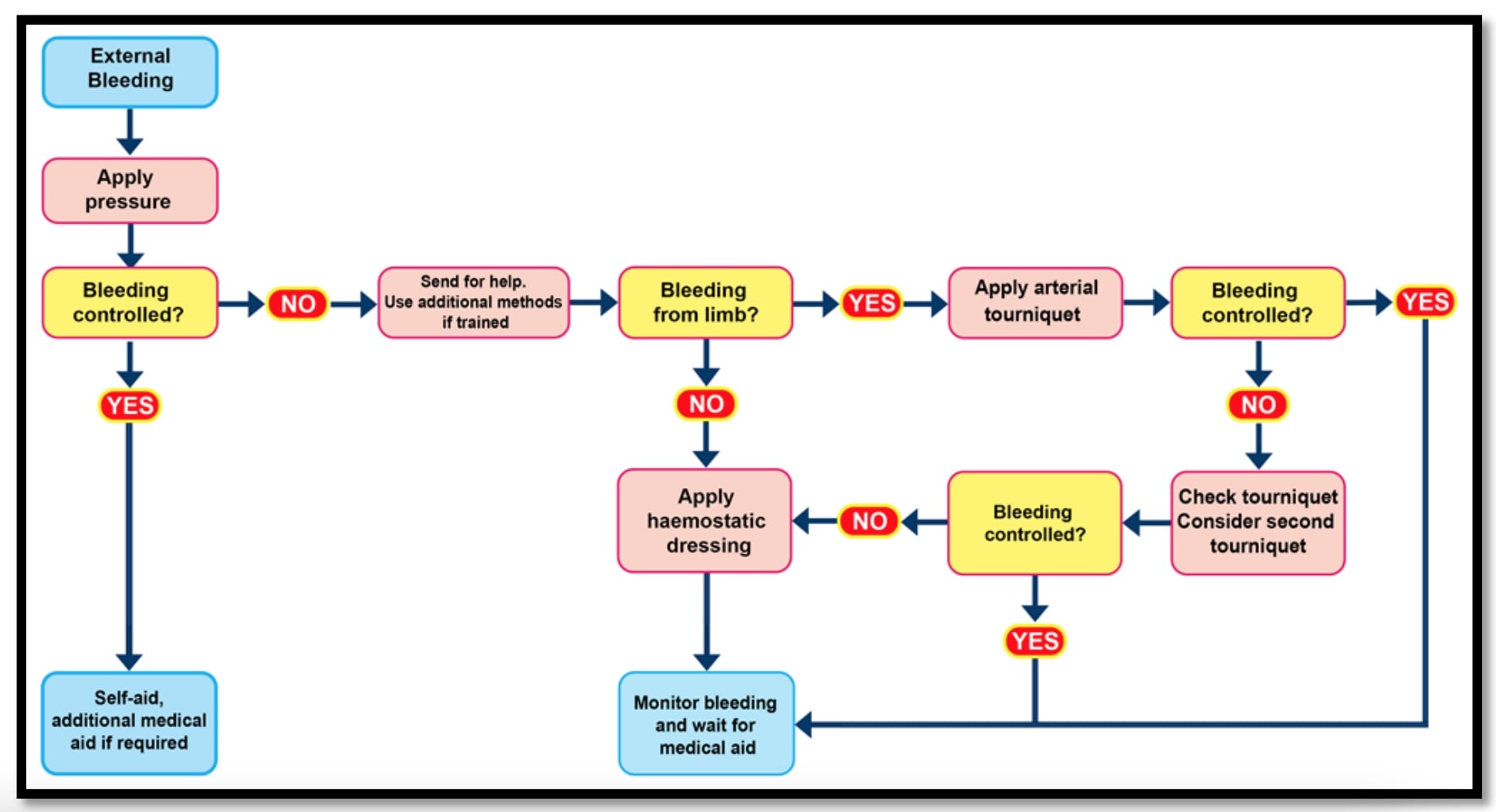
1.6 Flow Chart for First Aid Control of External Bleeding
2 Internal Bleeding
2.1 Recognition
Internal bleeding may be difficult to recognise, but should always be suspected where there are symptoms and signs of shock. [Refer to ANZCOR Guideline 9.2.3]
Internal bleeding includes bruising, locally contained bleeding (e.g. an 'egg on the head') and the bleeding associated with injury or disease of organs in the abdomen or chest, as well as fractures. Severe bleeding may also occur from complications of pregnancy.
Symptoms and signs may include:
- pain, tenderness or swelling over or around the affected area
- the appearance of blood from a body opening, eg:
- bright red and/or frothy blood coughed up from the lungs
- vomited blood which may appear bright red or as dark brown 'coffee grounds'
- blood-stained urine
- vaginal bleeding or bleeding from the penis
- rectal bleeding which may be bright red or black and 'tarry'
- shock in the case of severe bleeding
2.2 Management
Severe internal bleeding is life-threatening and requires urgent treatment in hospital.
- Send for an ambulance.
- Lie the person down
- Treat shock [Refer to ANZCOR Guideline 9.2.3]
2.3 Closed Bleeding in a Limb
- If there is bruising to a limb and no external bleeding, we suggest to use pressure and a cold pack if available.5 [CoSTR 2015: weak recommendation, low quality evidence]
- If closed bleeding in a limb is causing severe swelling or pain, or the person is showing signs of shock [Refer to ANZCOR Guideline 9.2.3], send for an ambulance [Good Practice Statement]
3 Nose Bleed (Epistaxis)
For a nose bleed:
- Pressure must be applied equally to both sides of the nose, over the soft part below the bony bridge (usually between the thumb and index finger).
- The person should lean with the head forward to avoid blood flowing down the throat.
- Encourage the person to spit out blood rather than swallow it as swallowed blood irritates the stomach, and causes vomiting which can worsen the bleeding.
- The person should remain seated at total rest for at least 10 minutes. On a hot day or after exercise, it might be necessary to maintain pressure for at least 20 minutes.
- If bleeding continues for more than 20 minutes seek medical assistance.
4 Management of All Severe Bleeding
- Call for an ambulance
- Reassure the person
- Assist the person into a position of comfort, preferably lying down
- Keep the person warm
- Monitor the vital signs at frequent intervals
- Administer oxygen if available and trained to do so [Refer to ANZCOR Guideline 9.2.10]
- Do not give any food or drink orally, including medications
- Treat shock [Refer to ANZCOR Guideline 9.2.3]
- If the person is unresponsive and not breathing normally, follow the Basic Life Support Flowchart [Refer to ANZCOR Guideline 8]
References
- Nathan P. Charlton, Janel M. Swain, Jan L. Brozek, Maja Ludwikowska, Eunice Singletary, David Zideman, Jonathan Epstein, Andrea Darzi, Anna Bak, Samer Karam, Zbigniew Les, Jestin N. Carlson, Eddy Lang & Robby Nieuwlaat (2020): Control of Severe, Life-Threatening External Bleeding in the Out-of-Hospital Setting: A Systematic Review, Prehospital Emergency Care, 2020, DOI: 10.1080/10903127.2020.
- Walker S.B., Cleary S., Higgins M. Comparison of the FemoStop device and manual pressure in reducing groin puncture site complications following coronary angioplasty and coronary stent placement. International Journal of Nursing Practice. Dec. 2001. 7 (6):366-75.
- Simon A., Bumgarner B., Clark K., Israel S. Manual versus mechanical compression for femoral artery hemostasis after cardiac catheterization. American Journal of Critical Care. Jul 1998. 7 (4):308-13.
- Naimer S.A., Chemla F. Elastic adhesive dressing treatment of bleeding wounds in trauma victims. American Journal of Emergency Medicine. 2000. 18 :816-819.
- Zideman, D. A., Singletary, E. M., De Buck, E.,et al. (2015). Part 9: First aid: 2015 International Consensus on First Aid Science with Treatment Recommendations. Resuscitation , 95, e225. http://www.cprguidelines.eu/assets/downloads/costr/S0300-9572(15)00368-8_main.pdf00368-8_main.pdf) Accessed 21/11/
- Devlin JJ, Kircher S, Kozen BG et al. Comparison of Chitoflex®, CELOX™, and QuickClot™ in Control of Hemorrhage. 2011. Journal of Emergency Medicine. 2011;41(3), 237- 245
Further Reading
- ANZCOR Guideline 9.2.3 Shock
- ANZCOR Guideline 9.1.4 Head Injury
- ANZCOR Guideline 9.2.10 The Use of Oxygen in Emergencies
About this Guideline
- Search date/s: ANZCOR search: October 2020
- Question/PICO: Population: Adults and children with severe, life- threatening external bleeding in an out-of-hospital setting. Bleeding from both compressible and non- compressible external sites were included. Nasal and oral bleeding were excluded.
- Intervention: All bleeding control methods applicable for use by trained or untrained first aid providers including manufactured or improvised tourniquets, hemostatic dressings or agents, cryotherapy, direct manual pressure, pressure points, pressure dressings or bandages, or elevation of the injured area.
- Comparisons: Direct manual pressure alone or any other management technique listed in Intervention, if a comparison was available. Outcomes: Outcomes were prioritized for importance a priori, as per the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach (Table 1).
- Study Designs: Randomized controlled trials (RCTs) and non- randomized comparative studies were included. If there were no or limited comparative studies, then case series of 4 or more subjects and simulation studies were also included. Conference abstracts and trial protocols were excluded. All languages were included where an English abstract was available.
- Method: Systematic Review (ILCOR First Aid Task Force, CoSTR) published April 20
- Primary reviewers: Finlay Macneil
- Other consultation: Nil
- Worksheet: See https://www.ilcor.org/
- Approved: April 2021
- Guidelines superseded: ANZCOR Guideline 9.1.1 - July 2017